Overview:
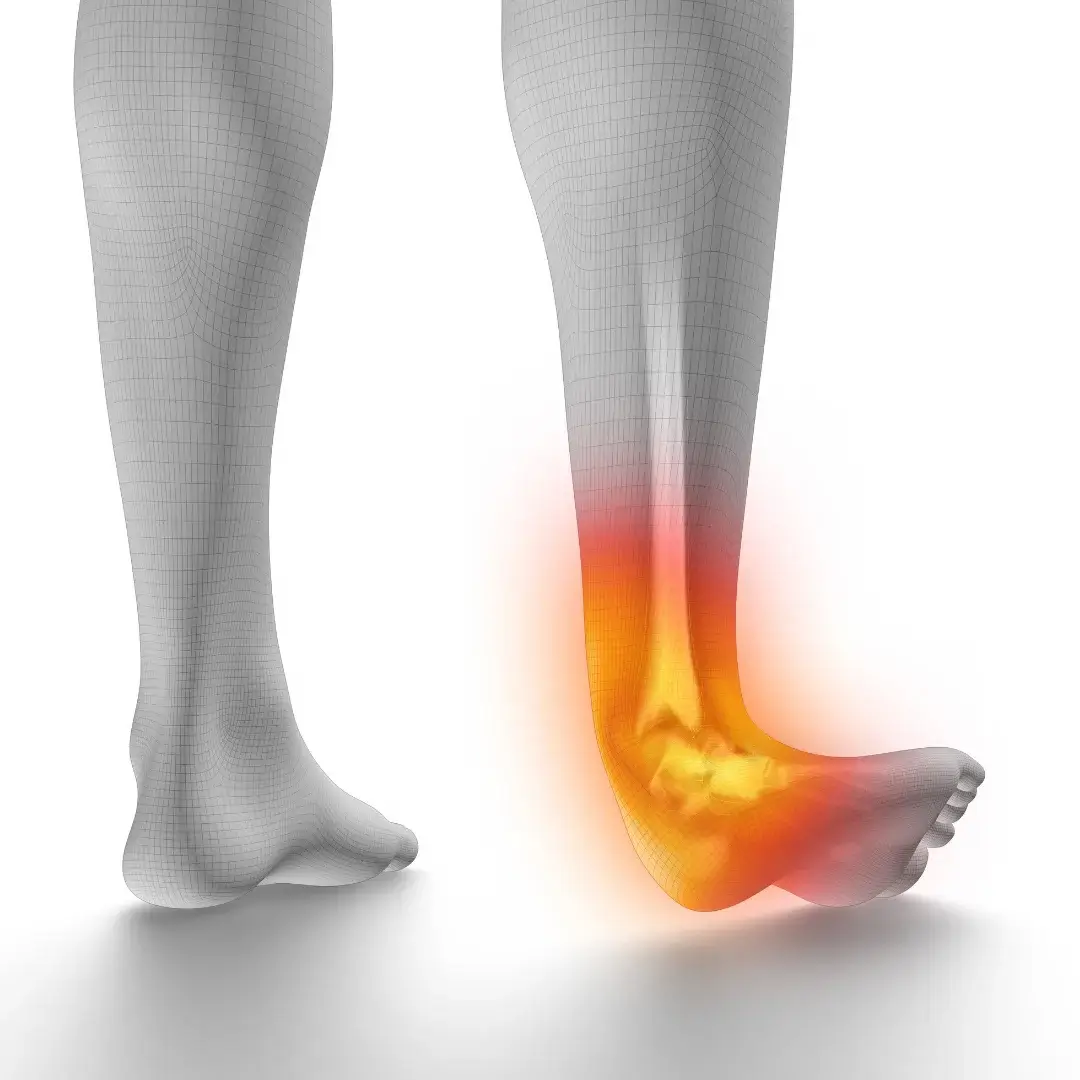
An ankle sprain is a common injury characterised by damage to the ligaments surrounding the ankle joint. It typically occurs when the foot twists or rolls beyond its normal range of motion, leading to stretching or tearing of the ligaments. Ankle sprains can range from mild to severe, depending on the extent of ligament damage, and may result in pain, swelling, bruising, and difficulty bearing weight on the affected ankle.
Anatomy:
The ankle joint is formed by the articulation of three bones: the tibia (shinbone), fibula (smaller bone of the lower leg), and talus (foot bone). Ligaments are strong bands of connective tissue that stabilise the joint and help prevent excessive movement. The most commonly injured ligaments in an ankle sprain include the lateral ligaments on the outside of the ankle (anterior talofibular ligament, calcaneofibular ligament) and the deltoid ligament on the inside of the ankle.
Causes:
Ankle sprains often occur during activities that involve sudden changes in direction, pivoting, or landing from a jump, such as:
- Sports-related activities (e.g., basketball, soccer, volleyball).
- Walking or running on uneven surfaces.
- Slipping or tripping on stairs or curbs.
- Accidents or falls.
Factors that may increase the risk of ankle sprains include inadequate footwear, muscle weakness or imbalance, previous ankle injuries, and environmental conditions.
Symptoms:
Signs and symptoms of an ankle sprain may include:
- Pain, particularly on the outer aspect of the ankle.
- Swelling and bruising around the ankle joint.
- Difficulty bearing weight or walking on the affected ankle.
- Instability or feeling of “giving way” in the ankle.
- Tenderness and warmth to the touch.
The severity of symptoms may vary depending on the extent of ligament damage, with mild sprains causing minimal discomfort and swelling, while severe sprains may result in significant pain, swelling, and functional impairment.
Treatment:
Treatment for an ankle sprain aims to reduce pain and swelling, promote healing of the injured ligaments, and restore function to the affected ankle:
- R.I.C.E. Therapy: Initial treatment often involves rest, ice, compression, and elevation (R.I.C.E.) to reduce pain and inflammation. Apply ice packs to the injured ankle for 15-20 minutes every few hours, and elevate the foot above heart level to minimise swelling.
- Immobilisation: In cases of moderate to severe ankle sprains, immobilisation with a supportive brace, splint, or walking boot may be necessary to protect the injured ligaments and prevent further damage.
- Weight Bearing: Gradual weight-bearing as tolerated is encouraged to maintain joint mobility and prevent stiffness. Crutches or a walking aid may be used initially to offload the injured ankle.
- Physical Therapy: A structured rehabilitation program comprising strengthening, flexibility, balance, and proprioception exercises is essential for restoring ankle strength, stability, and range of motion. Physical therapy may also include manual therapy techniques, such as joint mobilisation and soft tissue massage, to aid in the healing process.
- Medications: Over-the-counter pain relievers, such as ibuprofen or acetaminophen, may be used to alleviate pain and discomfort. Topical analgesic creams or gels may also provide temporary relief of pain and inflammation.
Prevention:
To prevent ankle sprains and reduce the risk of recurrence, consider the following preventive measures:
- Proper Footwear: Wear supportive shoes with good ankle support, cushioning, and traction, especially during physical activities or sports.
- Warm-Up and Stretching: Engage in a thorough warm-up routine before exercise or sports to prepare the muscles and ligaments for activity. Incorporate dynamic stretches to improve flexibility and range of motion.
- Strength and Balance Training: Include exercises that target ankle stability, strength, and proprioception (awareness of body position) in your fitness regimen. Focus on strengthening the muscles around the ankle joint, including the calf muscles, peroneal muscles, and intrinsic foot muscles.
- Gradual Progression: Gradually increase the intensity, duration, and frequency of physical activity or sports participation to allow the body to adapt and minimise the risk of overuse injuries.
- Environmental Awareness: Be mindful of environmental factors such as uneven terrain, slippery surfaces, or obstacles that may increase the risk of falls or ankle injuries. Use caution when walking or running on unstable surfaces.
- Protective Gear: Consider wearing ankle braces or supports during high-risk activities or sports, particularly if you have a history of ankle instability or previous sprains.
Outlook/Prognosis:
The prognosis for an ankle sprain depends on the severity of the injury, adherence to treatment, and rehabilitation efforts. Most mild to moderate ankle sprains heal within a few weeks with conservative management, while severe sprains may require a longer recovery period and rehabilitation program. Prompt and appropriate treatment, including rest, immobilisation, and physical therapy, can help minimise pain, swelling, and functional limitations, and promote a full return to activity. However, individuals with a history of recurrent ankle sprains or persistent instability may be at increased risk of future injuries and may benefit from targeted prevention strategies and ongoing rehabilitation. If symptoms persist or worsen despite conservative treatment, consult a healthcare provider for further evaluation and management.